62nd National Congress of the Italian Society of Rheumatology
Vol. 77 No. s1 (2025): Abstract book of the 62th Conference of the Italian Society for Rheumatology, Rimini, 26-29 November 2025
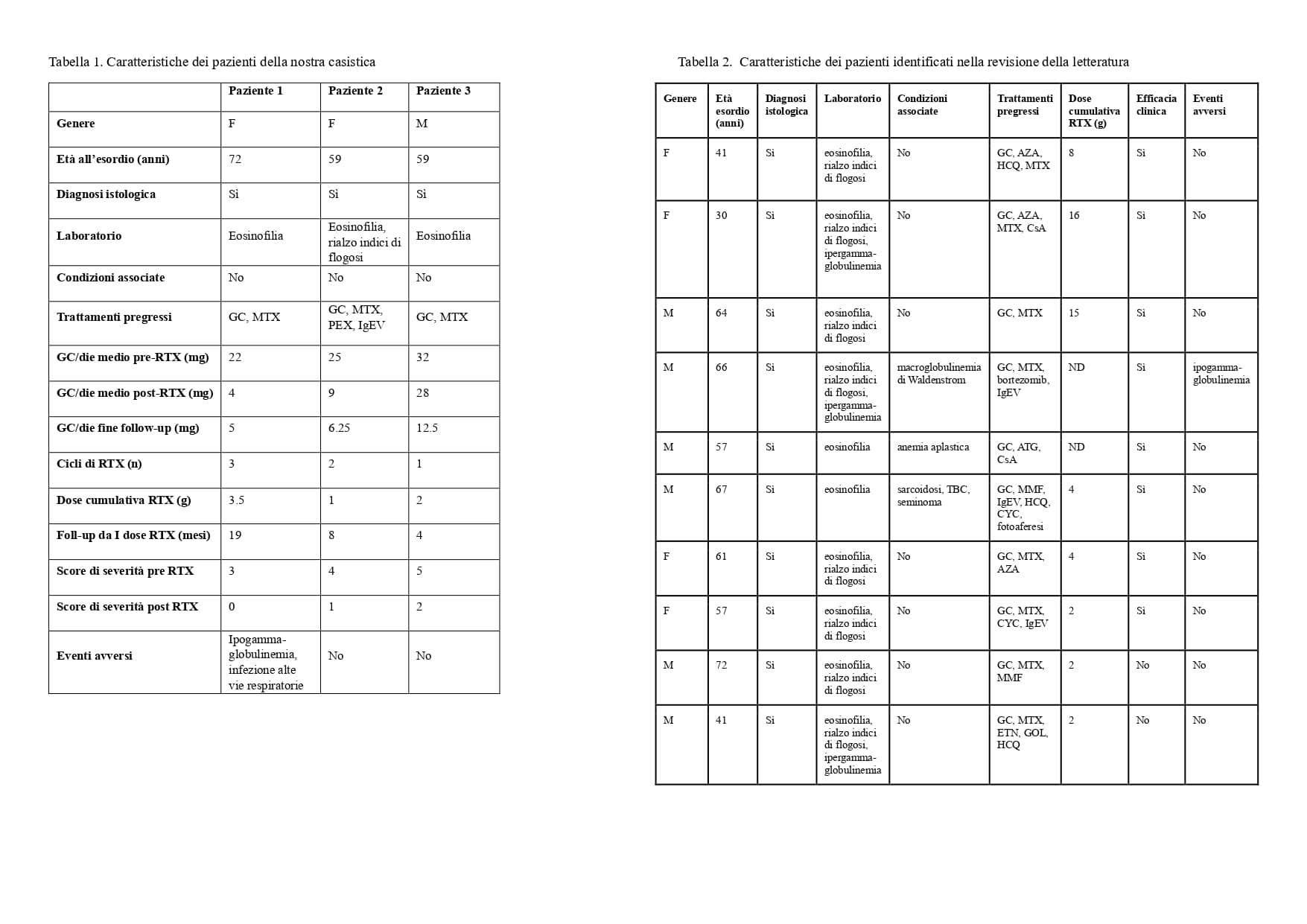
PO:33:203 | Efficacy and safety of rituximab in eosinophilic fasciitis: report of three cases and systematic literature review
Andrea Benini1, Beatrice Moccaldi1, Marco Binda1, Anna Cuberli1, Mariangela Favaro1, Andrea Doria1, Elisabetta Zanatta1 | 1UOC Reumatologia, Azienda Ospedale, Università di Padova, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 26 November 2025
112
Views
0
Downloads