62nd National Congress of the Italian Society of Rheumatology
Vol. 77 No. s1 (2025): Abstract book of the 62th Conference of the Italian Society for Rheumatology, Rimini, 26-29 November 2025
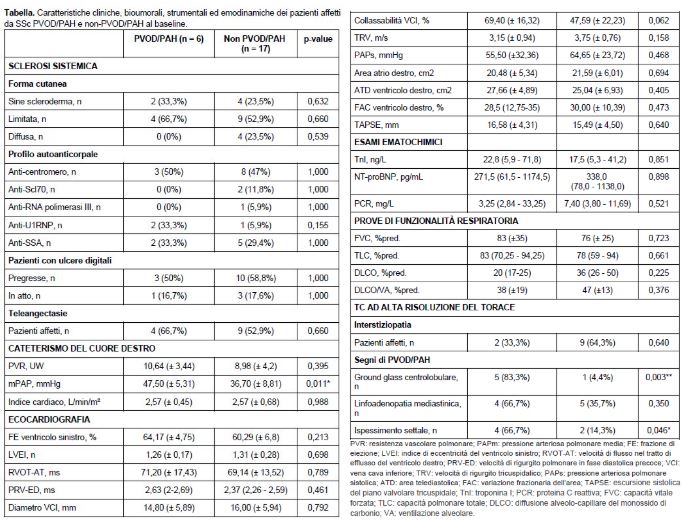
PO:32:180 | Clinical and hemodynamic profile of patients with SSC-PAH with and without pulmonary veno-occlusive disease: a single-center study
Anna Cuberli1, Michele Strosio2, Alessandro Magi2, Beatrice Moccaldi1, Marco Binda1, Andrea Benini1, Andrea Doria1, Martina Perazzolo Marra2, Giulia Famoso2, Laura De Michieli2, Elisabetta Zanatta1|2 | 1UOC Reumatologia, DIDAS Medicina Dei SIstemi, Azienda Ospedale Università di Padova; 2UOC Cardiologia, DIDAS Medicina Dei Sistemi, Azienda Ospedale Università di Padova, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 26 November 2025
72
Views
0
Downloads