62nd National Congress of the Italian Society of Rheumatology
Vol. 77 No. s1 (2025): Abstract book of the 62th Conference of the Italian Society for Rheumatology, Rimini, 26-29 November 2025
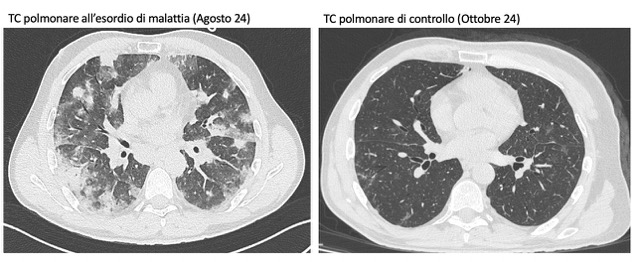
PO:22:039 | A rare form of interstitial lung disease: granulomatous and lymphocytic interstitial lung disease
Francesca Cozzini1|2, Francesco Falco1, Alberto Cavazza1, Lucia Spaggiari3, Chiara Marvisi1, Francesca Petrillo1|2, Caterina Ricordi1|2, Francesco Muratore1|2, Fabio Brandolino1, Ilaria Chiapparoli1, Carlo Salvarani1|2, Andreina Manfredi1|2 | 1IRCCS Policlinico San Matteo, UO di Reumatologia, Pavia; 2Università degli studi di Modena e Reggio Emilia, Modena, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 26 November 2025
82
Views
0
Downloads