62nd National Congress of the Italian Society of Rheumatology
Vol. 77 No. s1 (2025): Abstract book of the 62th Conference of the Italian Society for Rheumatology, Rimini, 26-29 November 2025
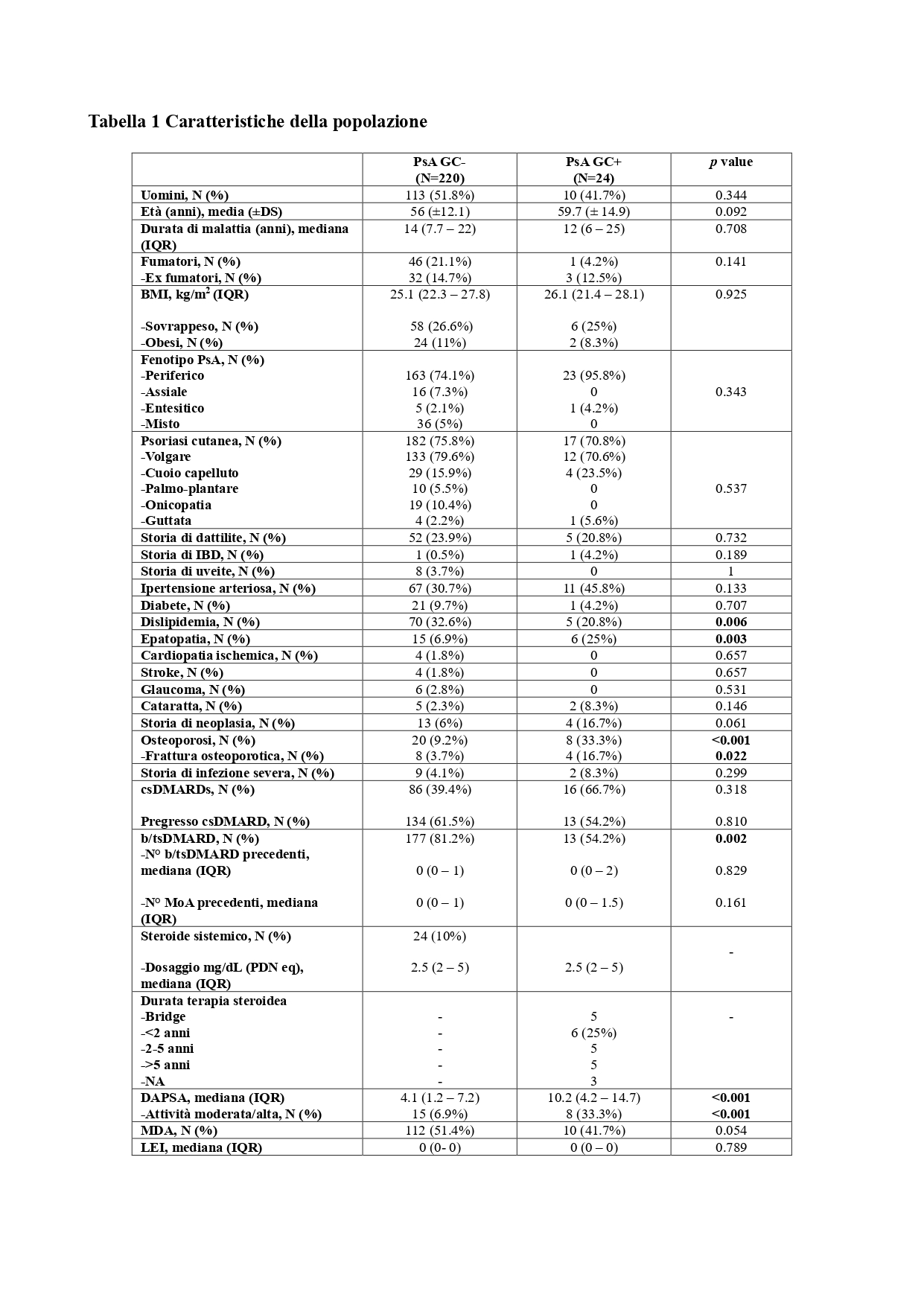
PO:02:023 | Monocentric analysis of systemic glucocorticoids in PsA: the art of balancing prescriptive appropriateness and risk factor management
Chiara Crotti1 2, Gilberto Cincinelli1, Giorgia Trignani13, Luca Ingrao13, Miriam Perino13, Roberto Caporali13 | 1Dipartimento di Reumatologia e Scienze Mediche - UOC Clinica Reumatologica, ASST Pini-CTO, Milano; 2Dipartimento di Reumatologia e Scienze Mediche - UOC Osteoporosi e Malattie Metaboliche dell Osso - ASST Pini-CTO, Milano; 3Dipartimento di Scienze Cliniche e di Comunità - Università degli Studi di Milano, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 26 November 2025
125
Views
0
Downloads