62nd National Congress of the Italian Society of Rheumatology
Vol. 77 No. s1 (2025): Abstract book of the 62th Conference of the Italian Society for Rheumatology, Rimini, 26-29 November 2025
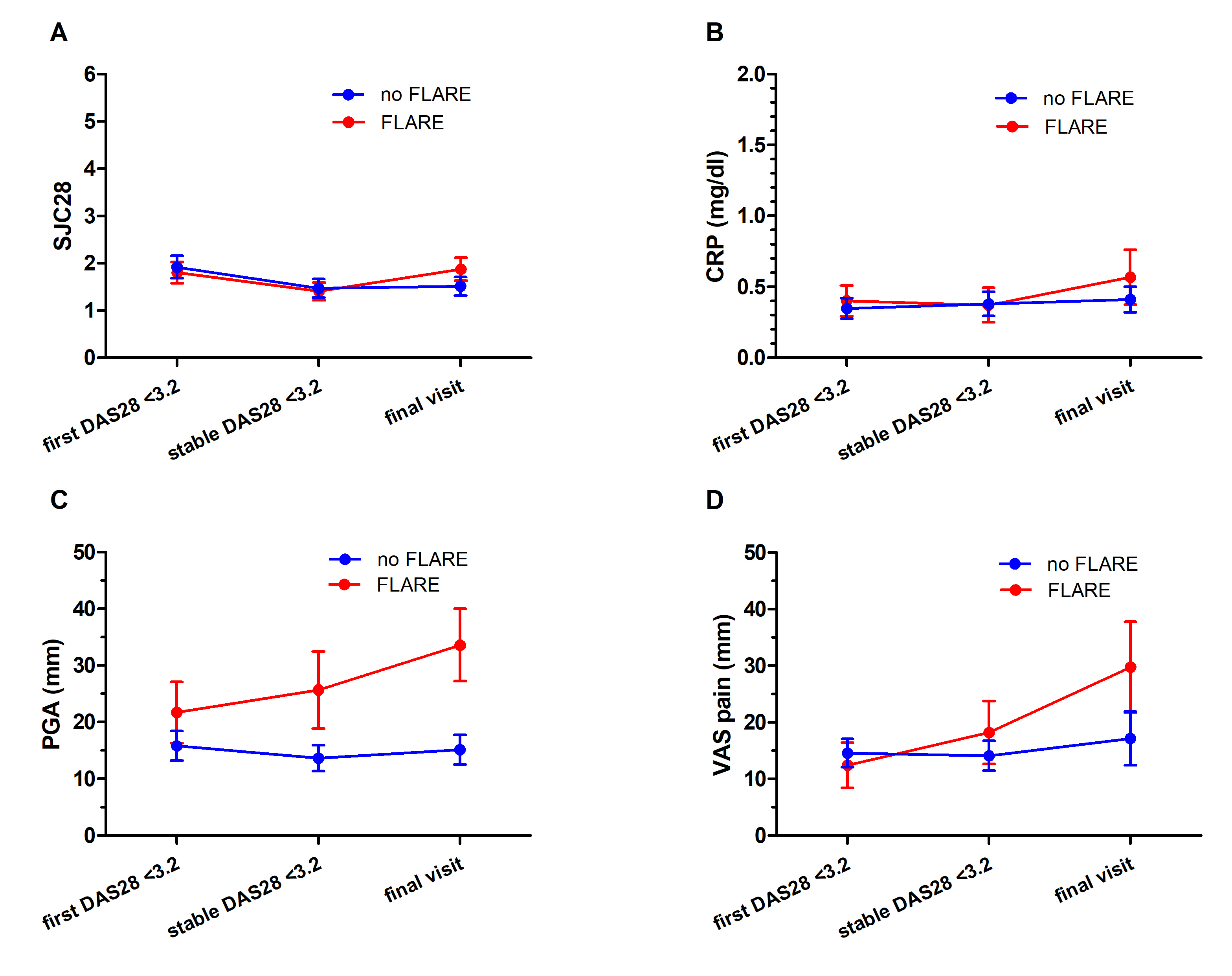
PO:07:111 | Worsening of patient-reported outcomes is an early predictor of disease flare in patients with rheumatoid arthritis in course of treatment with conventional synthetic disease modifying anti-rheumatic drugs
Ludovico De Stefano1|2, Federica Sabatelli1|2, Clelia Zampaglione1|2, Blerina Xoxi2, Antonio Manzo1|2, Carlomaurizio Montecucco1|2, Serena Bugatti1|2. | 1Department of Internal Medicine and Therapeutics, University of Pavia, Pavia, Italy; 2Division of Rheumatology, IRCCS Policlinico San Matteo Foundation, Pavia, Italy.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 26 November 2025
94
Views
0
Downloads