62nd National Congress of the Italian Society of Rheumatology
Vol. 77 No. s1 (2025): Abstract book of the 62th Conference of the Italian Society for Rheumatology, Rimini, 26-29 November 2025
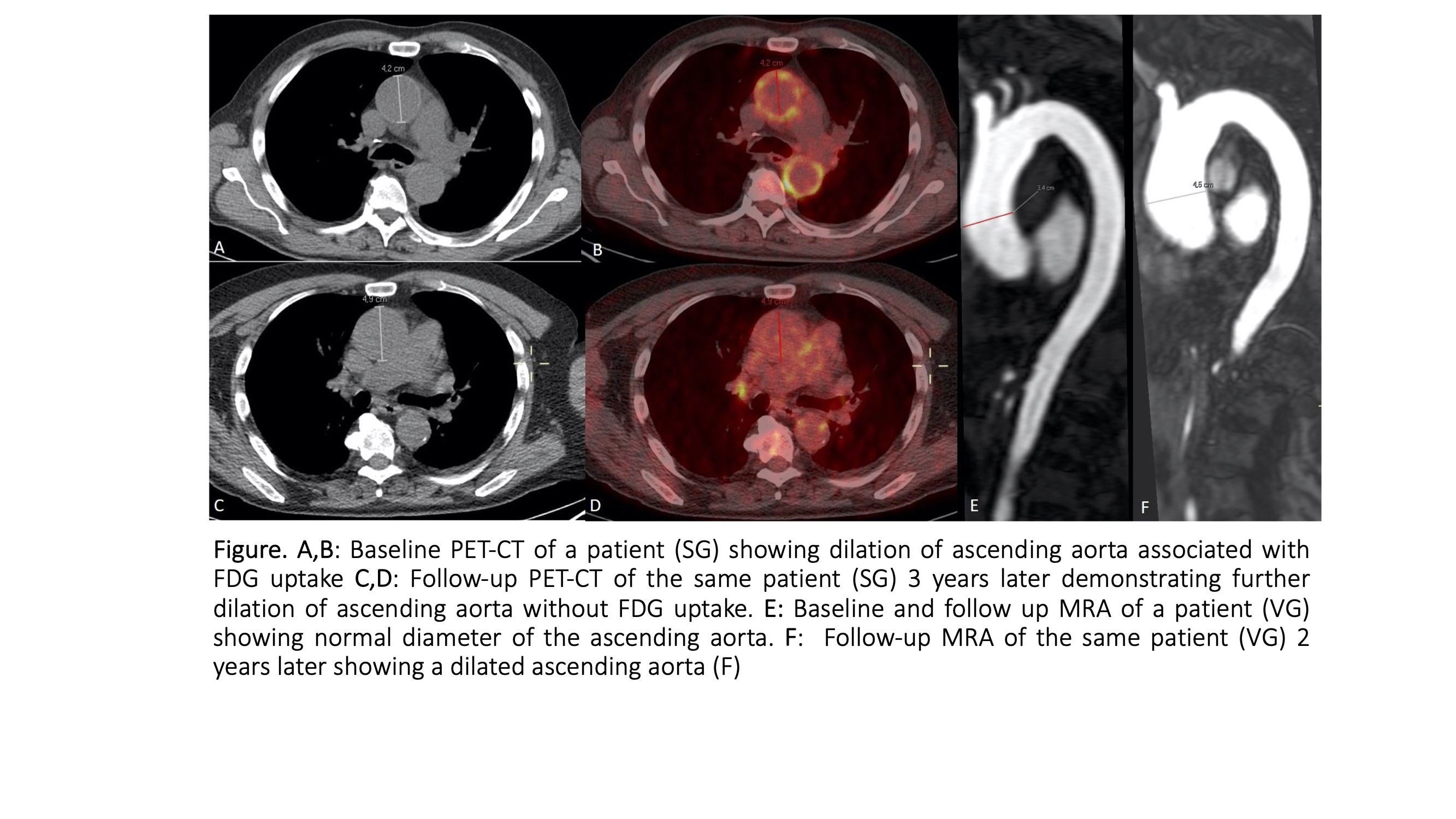
CO:12:5 | Aortic inflammation and aneurysm risk in giant cell arteritis: a multicenter imaging study
Caterina Ricordi1, Chiara Marvisi1, Konstanze V. Guggenberger2, Rudolf A. Werner3, Pamela Mancuso8, Giulia Besutti4, Sebastian E. Serfling5, Roberto Farì4, Matthias Frohlich6, Rexhep Durmo7, Michael Gernert6, Lucia Spaggiari4, Annibale Versari7, Paolo Giorgi Rossi8, Pierpaolo Pattacini4, Marc Schmalzing6, Carlo Salvarani1, Thorsten Bley9, Francesco Muratore1. | 1Rheumatology Unit, AUSL IRCCS di Reggio Emilia and Università di Modena e Reggio Emilia, Italy; 2Department of Diagnostic and Interventional Neuroradiology, University Hospital Wuerzburg, Germany; 3Department of Nuclear Medicine, University of Frankfurt, Germany; 4Department of Radiology, AUSL IRCCS di Reggio Emilia, Italy; 5Department of Nuclear Medicine, University Hospital Wuerzburg, Germany; 6Rheumatology and Clinical Immunology, Department of Internal Medicine II, University Hospital Wuerzburg, Germany; 7Nuclear Medicine Unit, AUSL IRCCS di Reggio Emilia, Italy; 8Epidemiology Unit, AUSL-IRCCS di Reggio Emilia, Italy; 9Department of Diagnostic and Interventional Radiology, University Hospital Wuerzburg, Germany
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 26 November 2025
93
Views
0
Downloads
Caterina Ricordi, Chiara Marvisi, Konstanze V. Guggenberger, Rudolf A. Werner, Pamela Mancuso, Giulia Besutti, Sebastian E. Serfling, Roberto Farì, Matthias Frohlich, Rexhep Durmo, Michael Gernert, Lucia Spaggiari, Annibale Versari, Paolo Giorgi Rossi, Pierpaolo Pattacini, Marc Schmalzing, Carlo Salvarani, Thorsten Bley, Francesco Muratore