Macrophage activation syndrome and rapidly progressive lung disease as life-threatening manifestations of anti-MDA5 antibody disease. A case report

All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
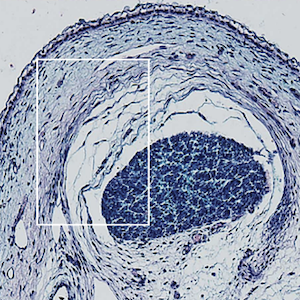
Anti-melanoma differentiation-associated protein 5 (MDA5) antibody-positive syndrome is a severe condition classified among the idiopathic inflammatory myopathies associated with rapidly progressive interstitial lung disease (RP-ILD). The present case report describes a complex patient with RP-ILD in the context of anti-MDA5-positive dermatomyositis (DM). The patient showed severe lung and skin manifestations involving hands, arms, and face, and the disease was first complicated by acute renal failure and then by macrophage activation syndrome (MAS). Finally, infectious risk delayed an effective treatment, probably increasing the rapid progression of lung involvement. A pathogenetic link between DM and MAS has been recently suggested; anti-MDA5 positive patients present higher serum soluble CD163 levels, which is a scavenger receptor for the hemoglobin/haptoglobin complex expressed on macrophages and a marker of macrophage activation in various conditions, including MAS. The patient has been treated according to the ACR/CHEST guidelines, adapting the strategy to his infectious complications. Beyond the complex clinical picture and treatment strategy, this case highlights the challenging decision-making process involved in the management of acute respiratory failure in patients with acute exacerbation of interstitial lung disease. The patient underwent helmet non-invasive ventilation (NIV), with a favorable clinical response. Helmet NIV has demonstrated advantages over mask interfaces, including better patient comfort, reduced air leaks, and more consistent delivery of positive end-expiratory pressure. These features contribute to lower inspiratory effort and improved clinical outcomes, including reduced intubation and mortality rates. In conclusion, patients with anti-MDA5 antibody disease need a multidisciplinary approach, including expert rheumatologists, pulmonologists, and radiologists for both monitoring and disease management.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.