ORAL COMMUNICATIONS - TOWARDS EULAR 2026 (I)
9 October 2025
2025: Prova Issue
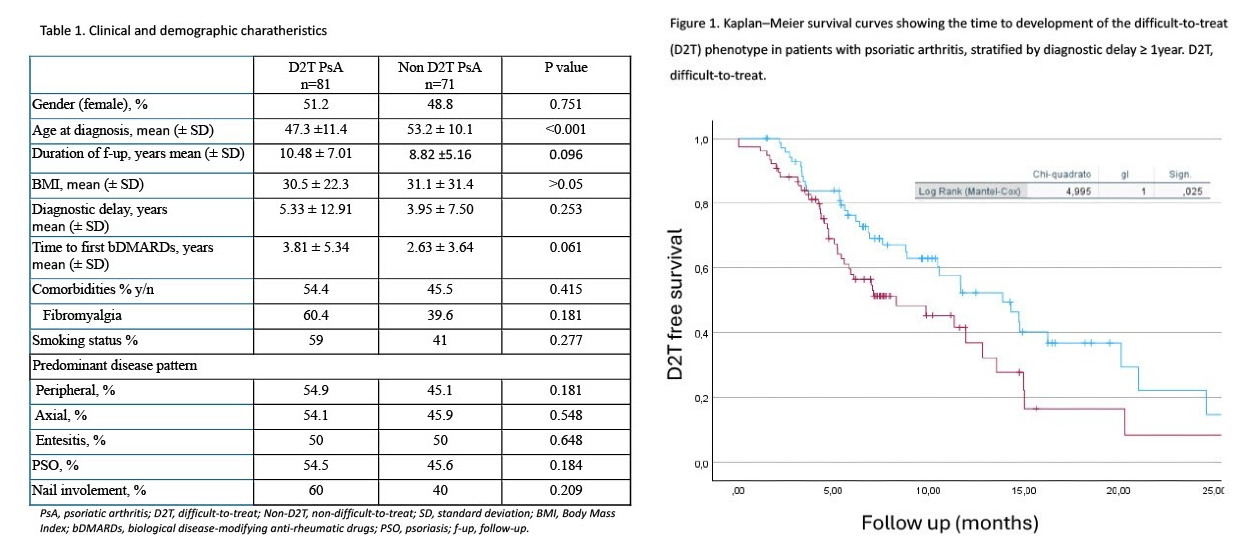
PO:02:017 | Difficult-to-treat psoriatic arthritis: clinical and ultrasonographic predictors in a real-life cohort
Federico Favaro, Elisa Bellis, Claudio Cruciani, Gloria Crepaldi, Valeria Data, Claudia Garulli, Claudia Lomater, Elena Marucco, Marta Saracco, Mariele Gatto, Annamaria Iagnocco. | Academic Rheumatology Centre, Departement of Clinical and Biological Sciences, University of Turin, AO Mauriziano, Torino, Italy.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
12
Views
0
Downloads