https://doi.org/10.4081/reumatismo.2023.1564
https://doi.org/10.4081/reumatismo.2023.1564
A case of Sjögren syndrome and anti-neutrophil cytoplasmic antibody-associated vasculitis
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
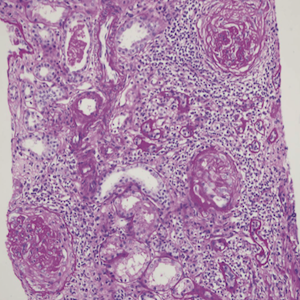
Sjögren’s syndrome (SS) is a rare disease with the highest reported prevalence of 0.01-0.09%. Anti-neutrophil cytoplasmic antibody-associated vasculitis (AAV) is another rare auto-immune disease (prevalence of 0.0009-0.01%). The co-occurrence of these two separate clinical entities in one patient might rarely be encountered as an overlap syndrome. Here, we present the case of a 60-year-old female patient who had complaints of headache, nausea, weakness, gritty sensation in her eyes, and dry mouth [unstimulated saliva production of 0.033 mL/minute (normal; >0.1 mL/minute)] with a blood pressure of 190/110 mmHg, hypertensive retinopathy, proteinuric kidney disease, positivity of myeloperoxidase anti-neutrophil cytoplasmic antibodies, anti-Ro-52, anti-Ro, and anti-La antibodies. Pauci-immune crescentic proliferative glomerulonephritis was found in a kidney biopsy and successfully treated with cyclophosphamide and methylprednisolone. The co-occurrence of these diseases was first reported in 1992 by Böttinger et al. Since then, nearly 37 cases of SS and AAV have been reported. By reporting this case of primary SS and AAV, we emphasize the importance of auto-antibody tests in searching for the etiology of patients with proteinuria.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.