Editorials
21 March 2023
Vol. 74 No. 4 (2022)
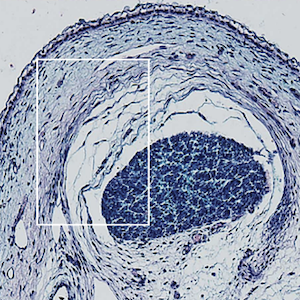
Emerging nailfold capillaroscopic patterns in COVID-19: from acute patients to survivors
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
774
Views
489
Downloads
Authors
Laboratory of Experimental Rheumatology and Academic Division of Clinical Rheumatology, Department of Internal Medicine, University of Genoa, Italy - IRCCS San Martino Polyclinic, Genoa, Italy.
Laboratory of Experimental Rheumatology and Academic Division of Clinical Rheumatology, Department of Internal Medicine, University of Genoa, Italy - IRCCS San Martino Polyclinic, Genoa, Italy.
Department of Internal Medicine and Department of Rheumatology, Ghent University (Hospital), Ghent, Belgium; Unit for Molecular Immunology and Inflammation, VIB Inflammation Research Centre, Ghent, Belgium.
Laboratory of Experimental Rheumatology and Academic Division of Clinical Rheumatology, Department of Internal Medicine, University of Genoa, Italy - IRCCS San Martino Polyclinic, Genoa, Italy.
The SARS-CoV-2 infection causing the Coronavirus disease-19 (COVID-19) is characterized by a broad range of clinical manifestations, implicating microvascular damage with endothelial dysfunction and different organ involvement.
Nägele MP, Haubner B, Tanner FC, et al. Endothelial dysfunction in covid-19: current findings and therapeutic implications. Atherosclerosis 2020;314:58-62. DOI: https://doi.org/10.1016/j.atherosclerosis.2020.10.014
Raghavan S, Kenchappa DB, Leo MD. SARS-CoV-2 spike protein induces degradation of junctional proteins that maintain endothelial barrier integrity. Front Cardiovasc Med 2021;8:687783. DOI: https://doi.org/10.3389/fcvm.2021.687783
DeOre BJ, Tran KA, Andrews AM, et al. SARS-CoV-2 spike protein disrupts blood-brain barrier integrity via rhoa activation. J Neuroimmune Pharmacol 2021;16:722-8. DOI: https://doi.org/10.1007/s11481-021-10029-0
Haberecker M, Schwarz EI, Steiger P, et al. Autopsy-based pulmonary and vascular pathology: pulmonary endotheliitis and multi-organ involvement in COVID-19 associated deaths. Respiration 2022;101:155-65. DOI: https://doi.org/10.1159/000518914
Cutolo M, Smith V. Detection of microvascular changes in systemic sclerosis and other rheumatic diseases. Nat Rev Rheumatol 2021;17:665-77. DOI: https://doi.org/10.1038/s41584-021-00685-0
Natalello G, De Luca G, Gigante L, et al. Nailfold capillaroscopy findings in patients with coronavirus disease 2019: broadening the spectrum of COVID-19 microvascular involvement. Microvasc Res 2021;133:10407. DOI: https://doi.org/10.1016/j.mvr.2020.104071
Sulli A, Gotelli E, Bica PF, et al. Detailed videocapillaroscopic microvascular changes detectable in adult COVID-19 survivors. Microvasc Res 2022;142:104361. DOI: https://doi.org/10.1016/j.mvr.2022.104361
Rosei CA, Gaggero A, Famà F, et al. Skin capillary alterations in patients with acute SarsCoV2 infection. J Hypertens 2022;40:2385-93. DOI: https://doi.org/10.1097/HJH.0000000000003271
Karahan S, Aydin K, Cetinkaya A, et al. Nailfold videocapillaroscopy in patients with COVID-19-associated pneumonia in intensive care units. J Coll Physicians Surg Pak 2022;32:455-60. DOI: https://doi.org/10.29271/jcpsp.2022.04.455
Çakmak F, Demirbuga A, Demirkol D, et al. Nailfold capillaroscopy: a sensitive method for evaluating microvascular involvement in children with SARS-CoV-2 infection. Microvasc Res 2021;138:104196. DOI: https://doi.org/10.1016/j.mvr.2021.104196
Ferrario CM, Jessup J, Chappell MC, et al. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation 2005;111:2605–10. DOI: https://doi.org/10.1161/CIRCULATIONAHA.104.510461
Monteil VKH, Kwon H, Prado P, Hagelkrüys A, et al. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell 2020;181:905–13. DOI: https://doi.org/10.1016/j.cell.2020.04.004
Koutsiaris AG, Riri K, Boutlas S, et al. COVID-19 hemodynamic and thrombotic effect on the eye microcirculation after hospitalization: a quantitative case-control study. Clin Hemorheol Microcirc 2022;82:379-90. DOI: https://doi.org/10.3233/CH-221554
Colonna C. Chilblain-like lesions in children following suspected COVID-19 infection. Pediatr Dermatol 2020;37:437-40. DOI: https://doi.org/10.1111/pde.14210
Fox SE, Akmatbekov A, Harbert JL, et al. Pulmonary and cardiac pathology in african american patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med 2020;8:681-6. DOI: https://doi.org/10.1016/S2213-2600(20)30243-5
Acquaro A, Brusca G, Casella S, et al. Evaluation of the oral microcirculation in patients undergoing anti COVID-19 vaccination: a preliminary study. Vaccines (Basel) 2022;10:1978. DOI: https://doi.org/10.3390/vaccines10111978
Bakakos P, Patentalakis G, Papi A. Vascular biomarkers in asthma and COPD. Curr Top Med Chem 2016;16:1599-609. DOI: https://doi.org/10.2174/1568026616666150930121157
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. DOI: https://doi.org/10.1016/S0140-6736(20)30183-5
Mostmans Y, Smith V, Cutolo M, et al. Nailfold videocapillaroscopy and serum vascular endothelial growth factor in probable COVID-19-induced chilblains: a cross-sectional study to assess microvascular impairment. Br J Dermatol 2022;187:1017-9. DOI: https://doi.org/10.1111/bjd.21785
Cutolo M, Soldano S, Smith V. Pathophysiology of systemic sclerosis: current understanding and new insights. Expert Rev Clin Immunol 2019;15:753-64. DOI: https://doi.org/10.1080/1744666X.2019.1614915
Smith V, Herrick AL, Ingegnoli F, et al. Standardisation of nailfold capillaroscopy for the assessment of patients with Raynaud's phenomenon and systemic sclerosis. Autoimmun Rev 2020;19:102458. DOI: https://doi.org/10.1016/j.autrev.2020.102458
Copyright (c) 2023 the Author(s)


This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.